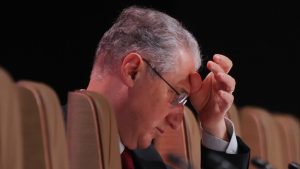
‘Dire’ NHS report shows scale of Sir Keir Starmer’s turnaround challenge
The dire state of England’s health service has been exposed in an official government-backed review of NHS services.
“The NHS is now an open book,” Lord Ara Darzi, the former health minister who led the independent investigation, concluded in his 142-page report. “The issues are laid bare for all to see.” Fixing the country’s broken vital public service may prove to be Labour’s biggest test.
While the UK Prime Minister Sir Keir Starmer has been clear that any additional funding for the NHS is conditional on reform, the uncomfortable assessments of Darzi will make it hard for ministers to ignore calls for extra cash.
The ‘missing billions’
The review sets out what the sector has been warning ministers for years. Health services have been hit by a decade of government austerity under which NHS spending grew at about 1 per cent in real terms, resulting in a “starvation of investment”.
A promise in 2018 to ensure spending on the NHS grew at a rate of 3.4 per cent a year was “broken”, the report stated. Instead, spending increased by just under 3 per cent a year between 2019 and 2024.
At the same time, England has spent almost £37bn less than peer countries on health assets and infrastructure since the 2010s, forcing the NHS to raid capital budgets in order to manage day-to-day spending.
This capital investment shortfall, which Darzi referred to as the “missing billions”, had hit productivity, left the service with crumbling buildings and led to a maintenance backlog of more than £11.6bn. Mental health services had been badly affected with patients being housed in “Victorian-era cells”.
Twenty per cent of the NHS estate predates the founding of the service more than 75 years ago. Staff had been left to work with “too many outdated scanners, too little automation and parts of the NHS are yet to enter the digital era”.
NHS budget ‘not spent where it should be’
Since 2006, successive ministers have pledged to move away from a hospital-centric approach and shift more care into communities. “In practice, the reverse has happened,” Darzi concluded.
The NHS budget was “not being spent where it should be” and too great a share was being “spent in hospitals, too little in the community, and productivity is too low”, he said.
Both levels of hospital expenditure and staff numbers have increased at a faster pace than other parts of the NHS.
The report showed how the number of community-based nurses declined by 5 per cent between 2009 and 2023, while the number of health visitors, who work with families after the birth of a child, fell almost 20 per cent over the period.
Improving preventive care within primary care services would help prevent conditions from advancing and would enable patients to be treated at an earlier stage before they required hospital admission. The distribution of funding over the past decade had made achieving this harder, the report showed.
Patients dying prematurely as waiting lists surge
One of the most damning conclusions reached by the cross-party peer was that thousands of people are dying too early as they wait to receive treatment.
Waiting times for hospital procedures had “ballooned” and overall waiting lists had swelled over the past decade. During the years of the Covid-19 pandemic, the NHS was forced to delay, cancel or postpone more routine care than any comparable health system.
Backlogs have contributed to an additional 14,000 deaths a year — “more than double all British armed forces’ combat deaths since the health service was founded in 1948”, according to the Royal College of Emergency Medicine.
Community care and mental health referral backlogs each stand at more than 1mn, while more than 100,000 children at present are waiting more than 12 months for access to mental health services. In hospitals, about 7.6mn are holding on for routine appointments while an estimated one in 10 patients are waiting more than 12 hours for A&E treatment.
“Long waits have become normalised”, the review concluded.
There were “appreciably higher” cancer mortality rates in England compared with other high-income countries. “No progress whatsoever” had been made to improve the early diagnosis of cancer between 2013 and 2021, while cardiovascular disease rates were also “going in the wrong direction”, said Darzi.
Declining health of a growing population
An ageing and growing population has irrevocably changed the demands on the NHS. The investigation warned that public health had “deteriorated”, with more people living with multiple conditions and for longer.
Housing standards, income and lifestyles were “moving in the wrong direction” and adding strain on an overstretched system, the report concluded. Those in greatest need had been most acutely affected, with 29 per cent of children living now in poverty.
An ageing population was the biggest driver of pressure on the NHS, while the deterioration of mental health services was also having an impact, Darzi concluded. The prevalence of depression had risen from 5.8 per cent in 2012 to 13.2 per cent a decade later.
NHS staff ‘disengaged’
Darzi uncovered worrying evidence that in the years since the pandemic, an overstretched workforce had resulted in staff becoming increasingly “disengaged”.
He found “distressingly” high rates of staff off sick, amounting to as much as one working month per year for every NHS nurse and midwife. Working conditions must improve, Darzi stated, not only to improve staff morale but productivity.
Labour’s plan to fix the health service
The government is set to publish its 10-year plan for the NHS next spring. Starmer has outlined three top priorities for reform: moving the NHS away “from an analogue to a digital” service; shifting more care from hospitals into communities; and “to be much bolder” with policies to prevent illness.
Despite falling outside the remit of the review, Darzi made a point of labelling the situation in social care as “dire”. The peer said a lack of funding had had “profound human cost and economic consequences” for elderly people and their families.
Speaking on Thursday, Starmer accepted it was not “possible to build an NHS for the future if we don’t fix social care as we do it”.
Despite being pushed on the timings for reforms, such as introducing a cap on the number of people who will pay for their care, the prime minister simply repeated his “ambition” to create a National Care Service.
#Dire #NHS #report #shows #scale #Sir #Keir #Starmers #turnaround #challenge